8 min read
October 14, 2025
FDA's DCT Guidance: Biotech Isn't Ready For It
FDA's DCT guidance promises transformation, but biotech need the digital infrastructure to deliver.
This month, FDA released the guidance snapshot for Conducting Clinical Trials with Decentralized Elements, a 6-page visual summary of the full September 2024 guidance designed to "increase public awareness and support efficient application." Translation: the rules are clear. Now the question is whether your company’s infrastructure can handle it.
The guidance covers the mechanics: remote visits, digital health technologies (DHTs), direct-to-patient IP shipment, local HCPs for routine tasks. The regulations haven't changed (21 CFR parts 312, 812 still apply), but FDA just handed biotechs a blueprint for trials that don't require patients to drive two hours for routine vitals. For oncology and specialty drug trials this could be transformative, if you've built the digital infrastructure to support it.
What This Guidance Unlocks
Let's start with what works. DCTs solve real problems that have plagued specialty drug trials for years:
Enrollment speed and cost reduction. By enabling remote visits and DHT monitoring, companies can reduce reliance on centralized sites, compress enrollment timelines, and cut operational costs. No more building out physical sites in every region. No more reimbursing patient travel for routine visits. Direct IP shipment to patients' homes streamlines logistics. For rare disease trials, where finding 50 evaluable patients can take 18 months, this is the difference between viable and impossible.
Access to the patients who matter most. Oncology trials have historically excluded rural patients, elderly patients with mobility limitations, and caregivers who can't take time off work for weekly site visits. The guidance explicitly supports leveraging local HCPs and telehealth to reach these populations. That goes beyond “diversity for compliance”. It's stronger real-world evidence that supports broader label claims and reduces post-market surprises. If your CAR-T trial only enrolled patients who could travel to academic medical centers, your safety and efficacy data doesn't reflect the real market.
Real-time data and adaptive designs. Explicit FDA support for DHTs (wearables, remote monitoring, continuous data capture) enables what traditional trials can't: real-time safety monitoring, adaptive dosing based on continuous biomarkers, and outcome tracking between scheduled visits. For oncology, where progression and adverse events don't wait for scheduled assessments, continuous monitoring could transform both trial efficiency and clinical utility.
This is the promise. Here's the catch: most biotech companies don't have the digital infrastructure to deliver it.
Digital Infrastructure Requirement Nobody's Discussing
Buried in the guidance snapshot's recommendations:
“Digital health technologies (DHTs) may allow transmission of data remotely and securely from trial participants wherever they are located. Sponsors should ensure that DHTs used in a DCT are available and suitable for use by all trial participants.”
That's not a suggestion. That's an infrastructure mandate. “Available and suitable for all participants” means:
• You're providing wearables or monitoring devices to patients who can't afford them
• Your DHT works for elderly oncology patients, not just tech-fluent millennials
• Data flows from patients' homes into systems that comply with 21 CFR part 11
• Remote data collection introduces variability you've planned for in your statistical analysis plan, not discovered when you try to lock the database
The guidance is explicit about limiting data variability: protocols must include specific instructions for remote activities, and sponsors should consider training or video supervision for at-home assessments.
That's not a telehealth visit. That's a digital infrastructure play that most small biotech teams aren't equipped to execute.
Where Digital DCTs Break Down
Companies read this guidance and ask “should we add remote monitoring of adverse events to our Phase 2 trial?” Wrong question. The right question is “can our systems handle decentralized data without compromising our ability to answer the regulatory question?” Here's where oncology trials specifically hit the wall:
The DHT integration problem. You're now managing data from wearables tracking patient activity, remote monitoring devices measuring vitals, patient-reported outcomes via mobile apps, local lab results from multiple facilities, and traditional site assessments, all feeding into a single database that FDA will inspect.
Take an oral oncolytic in metastatic disease. You want continuous monitoring of patient-reported symptoms between clinic visits. Sounds great until you're managing:
• DHT device distribution and technical support for 80 patients across 15 states
• Data transmission from patients' homes through a HIPAA-compliant platform
• Integration with your EDC system that was designed for site-based data entry
• Variability in reporting (some patients check symptoms daily, others weekly, some when they feel bad)
• 21 CFR part 11 compliance for all of it
Each data source is a new compliance risk. Pharma companies with validated data management platforms can absorb this. Biotech teams managing trials in Google Drive and Excel? This is where protocols fall apart.
The equity and access paradox. FDA's emphasis on “available and suitable for all participants” creates a catch-22 for resource-limited biotechs. The guidance pushes you to include rural and underserved populations, but providing devices, managing connectivity issues, and offering technical support for patients without reliable internet is an operational burden most small teams can't absorb. For an oncology trial targeting elderly patients with limited mobility, you need DHTs that don't require smartphones. You need local HCPs who can perform in-home assessments. You need direct IP shipment that maintains cold-chain integrity. That's not trial design; that's logistics infrastructure. The endpoint and analysis challenge. The guidance's focus on “limiting variability” is a warning: FDA expects your statistical plan to account for how remote data collection affects your endpoints.
Example: You're running a trial for an oral agent in advanced NSCLC. Traditional trial design: patients come to the clinic every 3 weeks for tumor assessments, vitals, and AE collection. DCT design: patients report symptoms via app, local HCPs perform monthly physical exams, imaging happens at local facilities.
Question: How do you ensure imaging quality is consistent across 20 local radiology centers? How does your independent review process work when scans come from multiple sources? How do you handle missing data when patients don't complete daily symptom reports? If you haven't designed your protocol and statistical plan to address this upfront, and if your data management system can't flag and resolve these issues in real time, you're building risk, not efficiency.
The Strategic Play: Infrastructure First, Design Second
Most companies will treat this guidance as a trial design decision: “Should we add DHTs to our next oncology protocol?” The smarter question: “Do we have the digital infrastructure to run a DCT without compromising data integrity or regulatory acceptance?"
Because the companies that win here aren't the ones that bolt on wearables at the last minute. They're the ones who built data management systems that can:
• Ingest remote data from multiple sources
• Maintain 21 CFR part 11 compliance across decentralized collection
• Flag data quality issues in real time
• Produce audit trails FDA will accept during inspection
That requires:
DHT selection based on your patient population, not the vendor pitch. For oncology trials with elderly patients, that might mean devices with large displays, simplified interfaces, and 24/7 technical support, rather than the slickest wearable with the best dashboard.
Data management plans designed for decentralization from day one. How does patient-reported outcome data flow from a mobile app to your EDC? Who validates remote vital signs? How do you handle variability in local lab reference ranges? If your answer is “we'll figure it out during the trial,” you're not ready.
Early FDA consultation on feasibility. The guidance recommends it. That's not optional language, it's a signal that they expect you to demonstrate you've thought through how decentralization affects your primary endpoint, your data quality, and your ability to answer the regulatory question.
What Biotechs Should Do Now
If you're designing an oncology trial in the next 12 months and considering decentralized elements:
Ask this first: Which trial activities genuinely require in-person assessments (complex imaging, infusions, detailed neurological exams), and which are we doing at sites because that's how we've always done it (vitals, patient-reported outcomes, routine labs)?
Then assess your digital readiness: Can your current systems handle remote data collection, DHT integration, and 21 CFR part 11 compliance? If your data management system is a CRO portal and Excel spreadsheets, you're not ready for decentralized data at scale.
Design for the patient population you need, not the one that's easy to reach: If your drug works best in elderly patients or rural populations that traditional trials exclude, DCT elements aren't optional, they're strategic. But that means investing in infrastructure that makes participation genuinely accessible, not just theoretically possible.
The promise of DCTs is real: faster enrollment, broader patient access, better real-world data, and potentially transformative trial efficiency for rare disease and specialty drugs. But the gap between promise and execution is digital infrastructure.
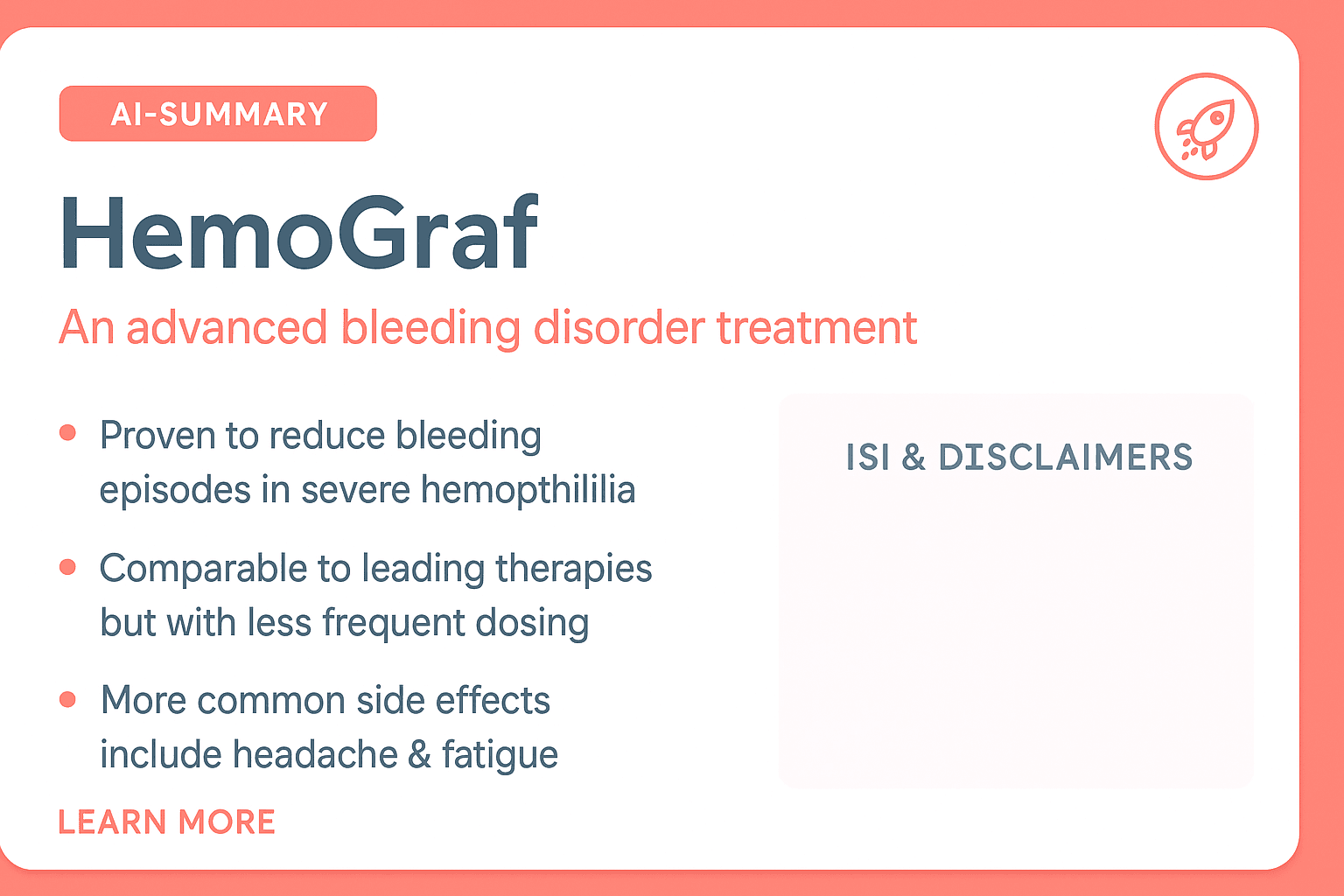
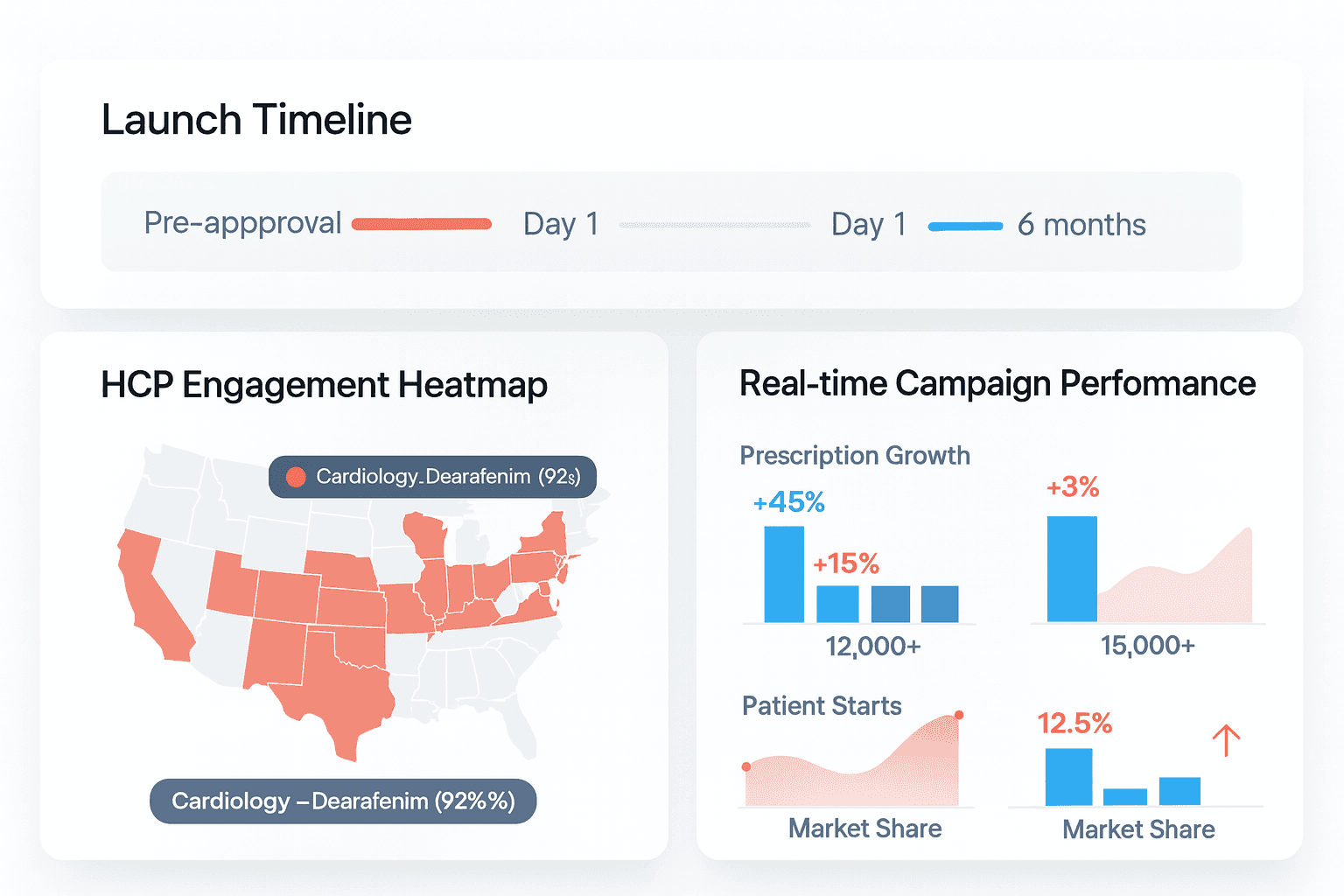
Launch Day 1. Build to Scale.
AI‑powered digital launch readiness: we compress months of work so your campaigns and infrastructure are live at approval and ready to grow with your portfolio.
10x Growth
Product adoption accelerated by digital innovation
15+ Years
Building digital engines for biotech and pharma
20+ Brands
Launches across oncology, rare disease & specialty